Hand Surgery
Hand Surgery has a share part in the plastic surgeries, which needs to be performed when the upper limbs are injured or if any disease occurs.
Hands have very delicate and important function, Even minor disruption of the hand integrity affects its functions and even leads to disability.
History
It is known that during World War II, thanks to the work Bunnella, the Hand surgery was established as a separate branch of science while its rise occurred in the 1960-70s with the development of microsurgery.

Photo 1 Bunella – One of the Founders of Hand Surgery and hit book “Surgery of the Hand” 1944г.
Using the microsurgical technique the segments of the amputated limb were replanted (Replantology), the missing fingers were restored using the auto transplants from the foot toes, microsurgical stiches of the hand nerves had been performed to restore senses in the fingers after the hand trauma ,as well as the elimination of soft tissue defects by transplanting the complex composition of vascularized segments.

Photo 2. Microscope and microsurgical instruments.
Hand surgery in Georgia was first established at our clinic when Mr. I. Kuzanov returned from Moscow to Georgia.Professor Kuzanov along with the talents of reconstructive-plastic and aesthetic surgery (post doctorate students at that time), R.S. Akchurin, N.O. Milanov, G. A. Stephanov, K.G. Abalmasov, T.I Peradze, and with the supervision of Professor V.S. Krilov established a micro surgery school.
With Prof. Kuzanov’s and G. Natsvlishvili’s leadership, an emergency microsurgical assistance department was established in Clinical Hospital No 1. More than 15,000 microsurgical operation had been conducted at the department. In 1982 Pofessor I. Kuzanov and G. Natsvlishvili were nominated for state honors in microsurgery.
Replantology
Replantology is part of the hand surgery, microsurgical techniques which allows replanting the amputated segments of a hand. To replant one finger o a hand the following procedures are necessary: attaching one artery and two veins , two nerves, as well as the tendon flexors and extensors, and restoration of bone integrity (osteo-synthesis) . Amputation of the forefinger of the hand results into losing the 80 % of hand functions.

Photo 1) Finger replantology conducted first in Georgia. Photos of the patient 3 months before and after the surgery.
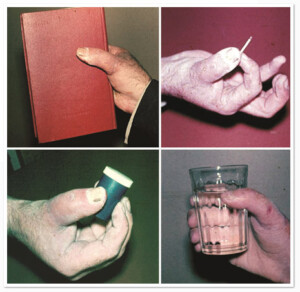
Photo 2) The patient with I amputated finger. Several months after the surgery the patient demonstrated adequate functional ability; both soft and hard functions of the hand are restored.


Photo 3) Glove-like (ring-like) amputation of the IV finger. The patient after 7 days and 3 months after the surgery.
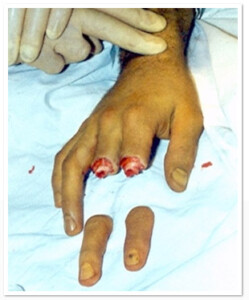

Photo 4) Guillotine type of amputation of II -III fingers. Before and one month after the surgery.

Photo 5) Guilliotine type amputation of (II-V) fingers/left hand. The surgery restored 4 arteries, 8 veins, 8 nerves, 8 muscles, and performed osteosynthesis of 4 wrist bones.

Photo 6) Amputation of II finger (2/3) and III-V fingers (fully) with one block. Replanatation of III-V fingers.
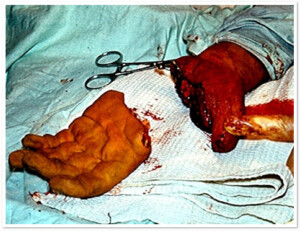

Photo 7) amputation of a hand at metacarparal level, before the surgery and 6 months after the surgery. Hand functions are restored.
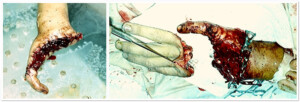

Photo 8 ) Amputation of right hand. The hand right after the surgery. The patient 25 years after the surgery. The functions of a hand are restored.
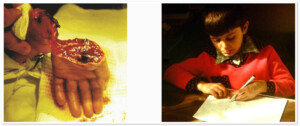
Photo 9) First time in the Soviet Union, replantation surgery of the hand was performed in Georgia in 1978. The patient was a 4-year old child. The photo shows the patient 6 months after the surgery with restored hand functions.


Photo10) amputation of the forearm at the lower end. The patient one year after the operations; functions are restored.

Photo11) Amputation of two hands. The patient 3 weeks after the surgery.

Photo 12) Amputation of the right forearm at the shoulder level. The patient after the operation with restored arm functions.
Finger Transplantation
It is known that the loss of fingers results into one’s disability, but the modern microsurgery achievements allow us to transplant fingers from one hand to another, or from one foot to another, thus enabling restoration of one’s employability.
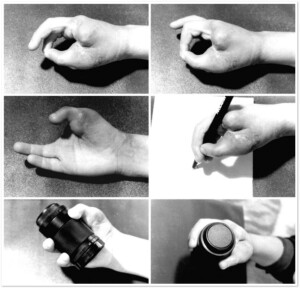
Photo.1) The patient with post-trauma amputation of I-III hand fingers. It is known that the loss of forefinger results into 80% disruption of hand functions. To restore hand functions, 2 fingers from the toes were transplanted to make the forefinger of a hand. The patient 6 months after the surgery. Hand functions are restored.
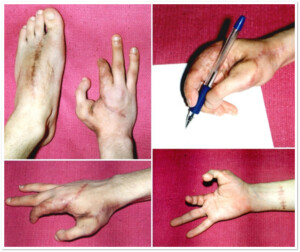

Photo 3) The patient with post-trauma amputation of the II hand finger at the level of proximal interphalangeal joints. Amputation of the III finger at the mid phalangeal segment. The patient cared much about the aesthetic side of the hand. To complete the restoration of the II right hand finger a stump were taken from the third finger of the left hand, which was used to lengthen the right palm stump. This has given an acceptable aesthetic result.



Photo 4 ) Patients with post-traumatic lesion of the right arm, III finger proximal interphalangeal joints. The patient was an artist and needed a complete restoration of hand function. In order to restore it to the 3rd finger of the right hand auto segment was transplanted: Vascularized tissue from the 3rd toe
A method has been developed and surgery has been conducted by prof. I. Kuzanov.
Congenial Defects
Polydactyly is having supernumerary fingers or toes. Politactyly occurs in one of 5000 infants. Most frequent form of polydactyly is having 6 fingers or toes on one hand or foot, however the number could reach 10 or more fingers/toes. Extra fingers/toes might possess all of the segments or part of the elements. Usually the extra fingers and toes only impede the regular functions of the limb s and has negative impact on the child’s psyche.
If the polydactyly of a hand is a cosmetic defect polydactyly of a foot disturbs the lower limb functions; Deformation increases with the child’s growth, which further complicates the correction of this anomaly. Foot defects hinder the process of walking, physical development and limit the choice of profession; Therefore, it adversely affects a child’s psyche, develops an inferiority complex .
Treatment of Polydactyly
This treatment of polydactyly is removal of unnecessary finger/toe through surgical intervention. In most cases, early intervention is carried out in the ICD . This is especially important during polydactyly of the foot. The child needs to have a regular foot shape before beginning to walk.
fore the child should have the right shape before the ankle began . The method of operation and the scale is determined based on individual cases as during the polydactyly other minor defects of the limbs are often observed.

Photo 1) A type of polydactyly, the patient has 6 toes on each foot.

Photo .2 ) Ulnar/Postaxial polydactyly, 6-toe foot before the operation and two months after the operation.
Syndactyly
Syndactyly is a complete or partial congenital fusion of fingers of the hand or foot, which causes cosmetic and functional defects, the disease occurs in about 10% of the newborns. There are various forms of syndactyl:
1 skin form – the adjacent fingers or toes are joined by thin skin, it is a relatively mild form.
- Skin-tissue form – in this case the adjacent fingers or toes are joined by skin and soft tissues;
- Endings form – in this case the connection is made only top phalangeal area of the fingers.
- Bone shape – in this case the phalangeal bones are connected, it is – one of the most complex form .
- Mixed form – this is the most difficult form and consists of various forms of syndactyly described above.
Syndactyly can be treated with surgical intervention. The operation devided the joined fingers/toes and the skin defects are correctd by the local plastic operation or skin grafting.
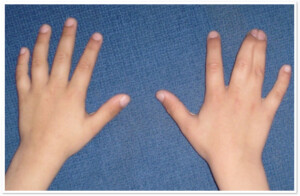
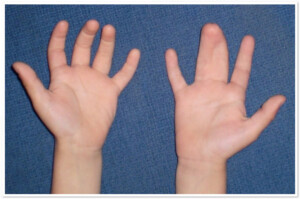

Photo 1) Bone Syndactyly of 3rd and 4th fingers and 4th and 5th toes.

Photo 2) Bone syndactyly of 4thand 5th fingers. The patient’s photo is one year from the surgery.
Gigantodactyly
This is a pathology when a finger/toe is much bigger than other fingers/toes. The pathology is usually congenital and can be carried over by inheritance. The treatment is a surgical intervention. In some cases it becomes necessary to amputate the finger/limb.
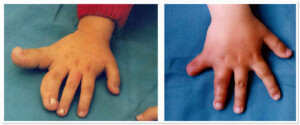
Photo 1) The patient with gigantodactyly of 4th and 5th fingers. The photos from before and 6 months after the operation.
Other Congenital Defects of the Hand
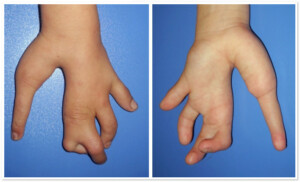

Photo 1) The patient with development anomaly of the hand (underdeveloped 4th finger, gap between the 3rd and the 4thfinger).

Photo 2) Congenital pathology of the 5th toe with short bending shape. Before and after the operation.
Post-burn contraction of limbs
As a result of the severe burns patients frequently develop post-burn contraction of the limbs. Post-burn contraction of the limbs is a limitation in the limb movement, which is expressed in inadequate opening and closure of the joints. Post-burn contraction usually limits the movement of joints due to the rough scars on the skin. In some cases post-burn contraction applies to joints and muscles. In the beginning stage the contraction can be treated by a comined conservative method: using various ointments, compression linen, physio therapy, massage and fitness.
However, in most cases (old scars) full treatment of the post-burn scars is achieved by surgical intervention, which involves removal of scars. Surgery is performed as a local plastic microsurgery, transplantation of the skin or using vascularized segments.

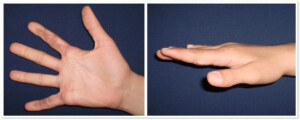
Photo 1) The patient with contracted fingers, 2nd and 5th finger of the right hand. Before the operation and 3 months after the skin transplantation.


Photo 2) The patient with contracted 1st finger after the burn. Before the operation and 1 month after the removal of the scar and the skin transplantation.

Photo 3) The patient with a contracted hand palm (with restricted finger movement). The patient before the operation and 6 months after the removal of the scar and skin transplantation.
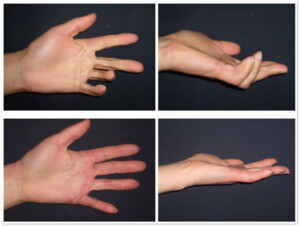
Photo 4) The patient with functional deformation of II-V fingers. Intraoperational slide after the removal of the scar. The defect was covered by skin segment.
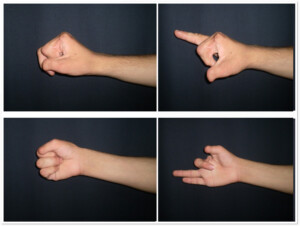
Photo 5a. The patient with lost 2 fingers after the detonator explosion in hand. The patient has III finger contraction.
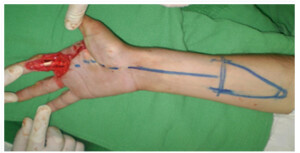
Photo 5B. Intraoperation slide. After the removal of the III finger scar, defect of the covering tissue developed, the defect was corrected by transplanting the skin from the arm segments.
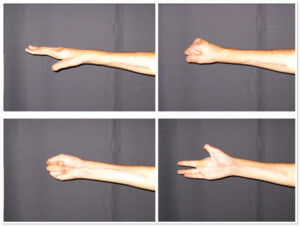
Photo 5c. The same patient after one year from the surgery.
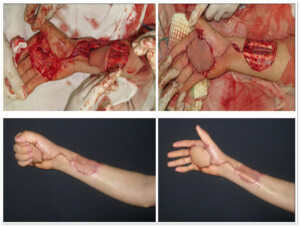
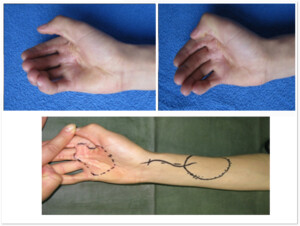
Photo 6)The patient with post-burn contracted hand palm, which limits the opening of the hand and fingers. Pre-surgery marking of the transplantation segments. Intraoperation slide, after removing the scars on the hand palm and transplantation of arm segments.


Photo 7)the patient with post-burn contraction of the right hand (“monkey hand”). The same patient 3 months after the removal of the scar and transplantation of the vascularized segment.

Photo 8A) The patient with thermal inurhy and functional disruption of the forearm, hand, muscles, joints and the skin.

Photo 8B) Soft tissue defect after removal of the scar. The surgery involved muscle restoration and covering the defects with free vascularized thoracodorsal segments. Blood movement is restored.

Photo 8c)The same patient 6 months after the surgery.

Photo 9A) The patient with post-burn Falkman contraction. The muscles for bending the fingers are damaged.
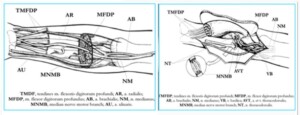
Photo 9B)To restore the functions of the arm, segments of the thoracodorsal were transplanted. Hand muscles were connected with the newly transplanted muscles.

Photo 9c)The same patient 6 month after the surgery.
Photo 10)The patient with post-traumatic two-head muscle defect on the right shoulder. The two-head muscle was restored by transplanting the thigh soft muscle. The patient one year after the surgery.

Photo 11a). The patient was inured in 2008 war after the bomb explosion. The patient developed a large-size bone-soft tissue defect.

Photo 11b)The remove the defect the first technique to be used was the reduction of the defect. At a second stage transplantation of the thoracodorsal segments was performed.

Photo 11c. The same patient 2 years after the operation. Functions of the limb are maintained.
During the post-burn syndactyly, usually the skin transplantation is indicated; in some cases transplantation of the vascularized segment is necessary.

Photo12) The patient with post-burn syndactyly and contraction of all toes, which impedes the walking functions. During the surgery the scars were removed and the skin has been transplanted, which improved the walking function.
Breast Restoration
Breast reconstructive surgery is associated with the oncology diseases of lactiferous glands. Therefore, breast restoration is a highly demanded surgery in the West.
Recent oncology surveys have shown that 12% of women suffer from breast cancer, with the number of cases doubled in the last 10-15 years. The mammography and ultrasonic tests have made early diagnostics of the lactiferous gland cancer possible, which has led to the organ sparing and preservation surgery.
The state of mind of a woman who has lost one or both breasts is truly horrible. Most of the women develop various psycho-neurological conditions caused by a malignant tumor and loss of a breast, an important part of womanhood. Women used to mask the defect by placing a special device in the bra. The outer fixation silicon prosthetic device used nowadays does not fully replace the breast.
The outer prosthetic device is hardly a good rehabilitation, especially for young women who find it awkward to reveal it. The reconstructive surgery aiming at provision of the prosthetic device closest to the female breast is the solution.
Breast reconstruction (restoration) can be achieved in three alternative ways:
- The lactiferous gland restoration by means of artificial materials (expander, implants);
- Breast restoration by the patient’s own tissues;
- The combination of the two implants plus the patient’s auto-transplanted tissues.
History
Breast reconstruction surgery has been an important target in the field of surgery for a long time. For example, in 1897 Iginio Tansini used the thoracodorsal segment rotation method during the radical mastectomy to cover the existing defect.
Holmstriom was the first to conduct the transplantation of Vascularized TRAM-segments (segments from abdominal straight muscles) in 1979. These segements can be reversed to the leg muscle to recover , although the majority of the specialists believe that this will disrupt the adequate blood supply of the segment, the result lacks the quality aestherically, and raises the risk of postoperative ventral hernia.
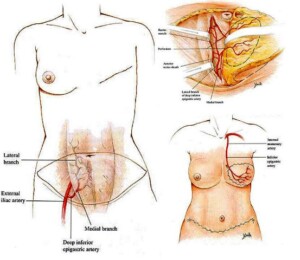
Koshima provided a DJEP segment from perforating blood vessels taken from the abdomen in 1989, which reduced the risk of hernia development and significantly reduces the post-traumatic effects of the operation.
Evolution of modern silicone implants that began in 1962, after Cronin and Gerow first used them for the breast augmentation, it became possible to widely use silicone implants and expanders in advanced breast reconstructive surgery.
Operation
Breast reconstructive operations in Georgia first started in our clinic in early 1990s. We use all three methods of breast reconstruction. The operation could be performed at one point during postmastectomy or can be deferred in several stages.
Single operations are carried out in our clinic together with leading oncologists and mammologists; Deferred breast reconstruction operations are coordinated and agreed with these specialists as well.
Reconstruction using the Implants
This method can be used in those cases where following the mastectomy there remains sufficient length of skin and subcutaneous tissue, and when a large breast muscles is maintained. In such cases the tissues can be increased by using expander dermotensia.
Expander is selected based on the healthy breast volume and size of the base. The implantation is performed in the area of mastectomy, considering the middle lines and sub-mammary wrinkes.
The volume of the expander increases through periodic injection of the solution and the tissues are being stretched out. Expander implantation can be perfomed in one or two stages.
In the first case, the so-called expander – implant is used. Once it reaches the required volume, the expander fills the role of the implant. In case of a two-stage operation, after the expander increases in volume, it it removed and the endoprotetis is implanted. These operations are technically quite simple and provided good cosmetic results; it’s less traumatic and postoperative rehabilitation period is shorter.
Breast Reconstruction using Autotransplants
This method has gained popularity in the recent 20 years, as the breast reconstruction using the auto-tissues is possible where expanders or implants cannot be implanted. Additionally, using this method provides better results aesthetically and ensures more acceptable shape of the breast and the results are permanent.
For the breast reconstruction surgery, different segments can be used for transplantation, though the most common ones are the skin segments from the thoracodorsal, skin and musle TRAM-segment and skin-facia DIEP- segment.
Reconstruction using the LD–segment
Breast reconstruction using the LD segment is indicated for patients with small and medium-sized breast. Spinal surgery is to recover from the side surface of the vascular thoracodorsal segment rotation into the chest. Taking the thoracodorsal muscle does not have harmful effects on the donor area.
Reconstruction using the TRAM–segment
This method is indicated for patients with medium and large-sized breast. Cannes – the muscular abdominal TRAM- segments are taken from the front surface fo the abdomen; it is made up of the skin – the fat layer of the abdominal muscles in the right part of it. Using the free vascularized TRAM- segments reduces the risk of ventral hernia, whereas such risk is much smaller compared to the rotation to the leg muscles.
The aesthetic result of this method is also much more acceptable.
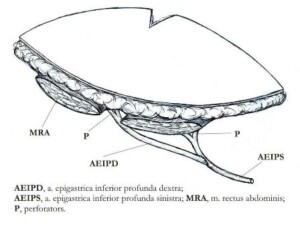
Reconstruction using the DIEP-segment
This method is indicated for patients with medium and large-sized breast. DIEP- segments are taken from the front surface of the abdomen, unlike the TRAM- segments, its composition is of skin-facia, which means that it does not use the muscle and therefore prevents the risk of hernia development. The two breast reconstruction methods, using TRAM and DIEP-segments allows to achieve two goals of breast restoration and abdominal reduction. . In July 2008, breast reconstruction using the DIEP-segments was first performed at our clinic in Georgia.
Phalloplasty
Construction and reconstruction of penis.
Urinary System surgery
Hipospodia, phimosis, restoration of virginity hymen, correction of genital labia.
Changing the Sex
Transforming the female into a male and vice versa.
Post-burn and post-trauma surgeries
Using vascularized segments
Reconstructive Orthopedy
Microsurgical treatment of false joints and bone defects
Surgery of congential lesions
Correction of cleft lip and palate